Tech Topic | November 2022 Hearing Review
A conversation with a teleaudiology specialist
By Sophie Brice, PhD, GradCert T&L, MSc, BMedSci (Hons) and Lisa Dyre, AuD
Studies have shown how remote support can potentially expand hearing health care to areas with minimal services,1,2 offer convenience and flexibility for both the provider and the client,3 and can provide care that satisfies the client – in particular, for aural rehabilitation follow-up.4 In response to client demand, some models of aural rehabilitative service delivery involve remote support from the start of the provider/client relationship. Sophie Brice is a pioneer in this area and shares some thoughts and tips from the trenches for those wanting to get started or expand remote support in their practice.
Lisa Dyre (LD): Hello, Sophie. Thank you for talking to us about remote support today. Tell us a bit about yourself and your passion for teleaudiology. You are really a bit of a pioneer in using remote support for rehabilitative hearing health care.
Sophie Brice (SB): I’m very passionate about remote support hearing healthcare. Having specialized in teleaudiology for over eight years now, I have accumulated a wealth of experience. I am delighted at the opportunity to share my experience with hearing care professionals looking to offer greater flexibility and remote support to their clients.
For me, remote support provision is the reality of modern hearing care. I live and work in Australia. Australia’s size, deregulation, and the limited access to health care in some regional areas make it geographically well-suited for telehealth. My work at Blamey Saunders Hears (BSH) allows me to reach clients who may otherwise not have services.
LD: Tell us a bit more.
SB: A client collaborative design has led to our successful remote support model. Blamey Saunders Hears (BSH) is an innovator in remote support hearing care and actually co-designed their teleaudiology services together with clients to ensure a model that would have appropriate self-education and self-reliance.5 So, for our practice, we have a strong suite of online tools and resources designed specifically for clients to test their hearing and gain more understanding of their hearing loss from their own homes. This includes a hearing loss questionnaire, hearing testing, and educational materials so that clients have the opportunity to make decisions about their hearing healthcare. For hearing care professionals getting started in teleaudiology, having online tools can be a good opportunity for offering client-centric hearing care.
LD: Is everyone a candidate for remote support?
SB: Potentially. However, we first address candidacy regarding health risks, instrument choice, and available client technology before continuing with remote support services. As I am not seeing the client in person, health risk is assessed using the Consumer Ear Disease Risk Assessment tool (CEDRA)6 that was developed specifically for use by online service providers to help determine candidacy for remote support. And then, I still rely on the same client medical history and information as I would for an in-clinic appointment.
LD: You mentioned technology. Research by Glista and colleagues,7 found that top concerns about performing teleaudiology were related to technology as well as whether the practice was audiology-centered and patient-centered. What are your thoughts on this?
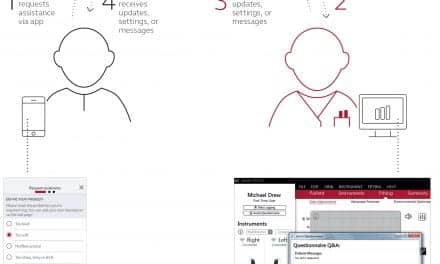
SB: Let’s start with the clinic technology. The bare necessities for remote support for any office boils down to what the clinic setup looks like. It’s likely that the technology is presently in place. Every clinic already has access to phone and email. Remote support for hearing aid products now mostly run from the user app, linked to proprietary software for the clinician. You do need to be comfortable with and knowledgeable about what you can do from your clinic using that software. Make sure you know how to plan, book, and initiate remote support with the products and setup you have. Look to your manufacturer for support. Phonak has a Remote Support Quick Start package (https://www.phonakpro.com/us/en/esolutions/digital-journey/overview.html#package) with downloadable resources (videos, implementation guidance, scheduling decision tree, and FAQ) to support you.
In terms of client interaction and Internet connections, if a client is first seen in the clinic, it is important to take the opportunity to check that they have their app in place and are able to work with it before they go home and try to use it alone. When this is not possible, make sure there is a plan in place for how to coach the client remotely. The plan could include videos, user guides, family assistance, as well as a teleaudiology appointment to help them. Having worked with a variety of remote support approaches over the years, I found it crucial to learn how to use each one from a user perspective. When you are comfortable with the client software, you can then decide what are the few most important things the individual client needs to be able to do.
And a word about the client’s personal technology: It is true that I cannot be an expert on every phone model and Bluetooth issue that exists in the world, however, I feel it is my responsibility to be comfortable and capable of working with the systems I offer as well as adapting to what the client uses and is willing to be guided on. It can be hard to keep up, but you can communicate closely with your team and manufacturer reps for support in acquiring new skills and knowledge. Also, admit to your clients that new technology brings new challenges for both of you. It is honest and appropriate to offer your best efforts to your clients. I believe they will always appreciate it even when you can’t give them an answer on the spot.
LD: Clinicians may worry about connections dropping when using remote support, is this a frequent problem? How do you handle it?
SB: Good question, because Internet coverage in Australia is not the best. This concern is another example of a practical factor you are faced with. If Internet stability is poor, plan to minimize any use of video, or maybe restructure your intended actions. For example, over a normal phone call, first talk a bit more about precisely what adjustment you may want to make, then use the remote connection to do that – and only that – with the given bandwidth, then save the session and close and resume by phone if needed. This really shouldn’t be the big barrier many people assume it will be; technical factors require forward and practical planning. Be ready to adapt and choose your next steps iteratively. From my desk in Australia, I have assisted clients in remote sessions in various locations, including outback Australia, and with people living on boats or camping.
LD: That does bring us to patient communication and interaction. Communicating over the Internet can be difficult for those with hearing loss. What thoughts do you have on this?
SB: It’s important to remember that clients are not trained in audiology or hearing aids, so do not always have the language or training to understand our counseling or to express what they are experiencing. Various studies have suggested we can do a better job when communicating with our clients in general. For instance, a 2019 literature review by Manchaiah et al8 found that audiologists dominated conversations and were not particularly patient-centered in their approach.
Personally, I rely on basic communication skills. I pay close attention to my choice of words and my pace of speech, and not just my volume. I leave clear gaps between sentences, use intonation to keep attention, and help indicate what information is key. I ask questions to keep them engaged and empowered. Asking questions is a skill that develops over time. You also get better at recognizing confusion or when clients are covering up the fact that they aren’t following you. It’s all really just using good communication skills that anyone would benefit from and providing an opportunity for client participation. My clinical colleagues have said they found their time working in teleaudiology was good skills practice for them and has helped them enhance their in-clinic communication skills.
LD: You mentioned candidacy and instrument choice. Can you elaborate?
SB: Sure. When addressing instrument choice, I think about what style or features will or won’t work for this client in their own home. Selecting a device that the client can comfortably manage independently should be handled exactly the same way whether the client is being fitted in a clinic or being assisted remotely. In my experience, clients may handle an aid perfectly in the office appointment but have more difficulty later and struggle with hearing aid management in their home. I believe that this real-time interaction is where remote support has some advantages in patient-centered care. It can make a difference in hearing aid use from the get-go.
LD: How do you address this specifically?
SB: In coaching a client who struggles with inserting or putting on the aids, we found that exchanging photos is great. Showing the ideal fit in a generic picture is nowhere near as effective as having them show you how they have put the hearing aids on at home on their own. We start with talking about the photos and coach them through the process.
The second strategy, which is also key, is to talk about what they feel when inserting them. Given that the client will be putting on the hearing aids on their own, unsupervised, daily, it is effective to coach them while allowing them to be in control, to teach them what to look for, what to feel for, and how they can tell what’s fitting well or not.
LD: In this digital arena, do you have any advice on offering digital reference materials for clients?
SB: I always am aware of what key support resources I should have ready for a particular client. There are dozens of web pages and user documents the client may find, so it will help you both to have a few preselected support documents to ask the client to focus on before they venture any further.
As mentioned earlier, getting to know your chosen hearing aid products now means getting to know the remote support capabilities in their apps. It can serve you well to have images and helpful links ready to send by email, especially if these are for helping the client get used to where certain features can be found on their app while they are still in the learning stage. Every time I realize that I am repeatedly pointing out the same detail, I prepare an annotated go-to image or email template to send, making my use of time far more efficient. Some other interesting tools you may want to add to your tool kit could be preferred sources of information on specialist topics like tinnitus, vestibular issues, or even at-home testing for speech or self-report topics. User-centric tools for gathering and sharing information are a great step forward in providing clinically guided resources that can help clients at any point of their hearing care journey.
I am confident that over time, more tools will be developed that will allow for a truly personalized hearing journey.
LD: Do you have any pragmatic advice for structuring your day when doing remote support?
SB: In my experience, remote support can be very efficient and patient focused whether it is used for all aspects of hearing care from the very first point of contact, or as a complementary service to traditional care. If a clinic is providing only remote hearing care, they can schedule the appointments as you might for traditional hearing care. For clinicians using a hybrid model of in-person/remote support, I do advise keeping a section of each workday or week reserved for remote support appointments.
Remote support can reduce the amount of time needed in face-to-face appointments. With traditional clinical care, we typically have contact with clients in a specific order: initial meeting, testing, discussion or fitting of hearing aids, and reviewing a hearing aid fitting. Remote care supports the iterative contact by allowing dynamic continued support – specifically addressing an individual client’s ongoing needs. Next teleaudiology steps for a client might include a clinician remote support call at an appointed time to check client progress on coaching points, or just a clinician follow-up phone call to quickly check in with the client, or perhaps, that proactive client contact may now stop until the client expresses further needs. Dynamic and adaptive support can be much more client friendly, and office efficiency can be increased by allowing providers to focus their time more effectively on clients who need more help while allowing self-sufficient clients to simply request help when they need it.
LD: How long do your appointments last?
SB: We generally book two types of appointments: 1) Phone call, 2) Adjustments. Phone calls help cover a lot of ground in clarifying things or discussing progress on an issue the client has been coached or guided on, or to gauge if further help is still needed. Our typical appointment time is 15-30 minutes, depending on what is needed. For hearing aid adjustments, all run through myPhonak app and Target. If we know ahead of time what we will be focused on or what particular adjustments we may be targeting, we may only book 30 minutes. For hearing aid adjustments, where we need to allow for additional support and coaching time, we will usually book a longer session.
LD: Sophie, thank you for your insights. Any last thoughts?
SB: As a teleaudiology specialist, the biggest part of my role has always been to adapt and respond to clients. Whether we are conducting traditional in-person appointments or providing remote support, a one-size-fits-all approach is not really client centered. Adapting how we provide care so that it is both iterative and dynamic, is a step toward appreciating that clients are in charge of their own care. They are also adjusting and adapting to their hearing care needs through practice and in their own personal way.
I believe that remote support is, above all, the strongest approach to truly reach more people looking to take action regarding their hearing.

Citation for this article: Brice S, Dyre L. Remote support for hearing health care: Thoughts from the trenches. Hearing Review. 2022;29(11):7-9.
References
- Swanepoel DW, Clark JL, Koekemoer D, et al. Telehealth in audiology: The need and potential to reach underserved communities. International Journal of Audiology. 2010;49(3):195-202.
- Coco L, Titlow KS, Marrone N. Geographic distribution of the hearing aid dispensing workforce: A teleaudiology planning assessment for Arizona. American Journal of Audiology. 2018;27(3S):462-473.
- Muñoz K, Nagaraj NK, Nichols N. Applied teleaudiology research in clinical practice during the past decade: A scoping review. International Journal of Audiology. 2021;60 (S1):S4-S12.
- Arnold ML, Schwartz B, Neil H, Chisolm TH, Sanchez, VA. Feasibility and assessment of a hybrid audiology service delivery model for older adult hearing aid users: A pilot study. American Journal of Audiology. 2022;31(3s):892-904.
- Saunders E, Brice S, Alimoradian R. Goldstein and Stephens Revisited and Extended to a Telehealth Model of Hearing Aid Optimization. In: Research Anthology on Telemedicine Efficacy, Adoption, and Impact on Healthcare Delivery. IGI Global; 2021:296-318.
- Klyn NAM,, Kleindienst RS, Bogle J, et al. CEDRA: A tool to help clients assess risk for ear disease. Ear and Hearing. 2019;40(6):1261-1266.
- Glista D, O’Hagan R, Moodie S, Scollie S. An examination of clinical uptake factors for remote hearing aid support: A concept mapping study with audiologists. International Journal of Audiology. 2021;60(S1):S13-S22.
- Manchaiah V, Bellon-Harn ML, Dockens AL, Azios JH, Harn WE. Communication between audiologist, patient, and patient’s family members during initial audiology consultation and rehabilitation planning sessions: A descriptive review. Journal of the American Academy of Audiology,.2019;30(9):810–819.