Cover Story | April 2014 Hearing Review
It’s time we all become committed to establishing a new social norm in hearing care—one that focuses on “maximal hearing and listening”
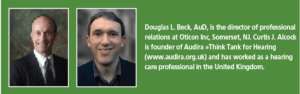
By Douglas L. Beck, AuD, and Curtis J. Alcock
There are some 35 million people in the United States with hearing loss.1 Amlani and Taylor2 reported market penetration has previously been thought to be 20% whereas MarkeTrak VIII3 assumed market penetration was closer to 25% (based on 8.2 million hearing aid users and some 33.4 million people with hearing loss). Of note, Amlani and Taylor2 reported perhaps only half of those with demonstrable hearing loss actually have a compelling need for amplification (in conventional audiological terms, consider a patient with normal thresholds from 250 to 6000 Hz and a 40 dB loss at 8000 Hz, or perhaps a patient with normal thresholds from 250 to 8000 Hz, but a 40 dB notch at 750 Hz). Therefore, one might argue market penetration is as high as 50%. Nonetheless, that still leaves an enormous pool of patients (50%) with significant hearing loss without amplification! (Also see Barbra Timmer’s article about mild losses in this edition of HR.)
This article focuses on considerations related to how to present amplification to hearing aid candidates, such that we facilitate effective and appropriate change to the social norm.
The Status Quo
The majority of people with significant hearing loss and/or who have difficulty understanding speech in quiet or noise appear to avoid hearing aid amplification. The traditionally accepted—and often quoted—time lapse between a person noticing a reduction in hearing (and/or listening ability) and subsequently acquiring a professional consultation and/or acquiring hearing aids is seven long and frustrating years. Of course, some people seek amplification sooner and some delay longer. However, “seven years” appears to be the average “lag time” for those who acquire amplification.
Once this person with hearing-impairment finally seeks professional consultation, the hearing healthcare professional (HHP; note we’ll use “HHP” to refer to the practitioners, the industry, and the associations) must often address and dispel the negative attitudes and impressions brought into the consultation room.
Indeed, widespread negativity associated with hearing aids is indicative of an underlying social norm, which views hearing healthcare (at best) as generally irrelevant and (at worst) as a threat.
As professionals, we often find ourselves simply accepting this state of affairs and, by default, responding in a manner that unintentionally reinforces the social norm. For example, we (in general) assure society we can hide the technology, and in doing so we affirm that using hearing aids—and, by inference, having hearing loss—is something to be hidden, or ashamed of, or embarrassed by.
Thus, the attitudes of society and the messages from the HHPs become locked into a vicious, negative, self-defeating circle.
The Goal
The goal of this article is to offer analysis and suggestions as to how we might break this self-perpetuating negative pattern by introducing a systematic framework designed to ultimately change the social norm. Central to accomplishing this goal is the identification of key stages at which hearing healthcare has the opportunity to become relevant to the public, while assuring the information provided facilitates positive images and attitudes. The specific goal might best be described as “maximal hearing and listening.”
Attitudes
Research into attitudes such as “The Elaboration Likelihood Method”4,5 and the “Heuristic Systemic Model”6 reveals people formulate their attitudes differently depending on how personally important or relevant a topic is. The less involved someone is, the more they rely on mental shortcuts (or heuristics) in formulating their attitude. Heuristics might facilitate a “follow the crowd” or perhaps “follow the experts” scenario. Indeed, they may consider (and ultimately base their opinion on) reasonably shallow questions such as “Does this make me feel good?” and perhaps “How attractive is the person telling me this?” However, as they become more involved, they likely become more willing to “do their homework,” dig deeper, consider, weigh pro-and-con arguments, and examine the evidence.
Therefore, to address the underlying social norm across the spectrum, the messages we (HHPs) present to society must facilitate positive and beneficial messages to those who do not believe hearing aids are currently relevant to them, and to those for whom hearing aids may already be relevant. Many of the people who currently consider hearing aids relevant have come through a process of change. So, one might argue, what we should focus on is “preparing the unready” for a time at which they become ready. That is, we must facilitate strategic and well thought through ideas and images that are truthful, positive, and “sticky” (ie, ideas that cling to you).
Further, the way in which the information is presented is of enormous consequence. “Framing” and “Priming” are two examples of how the presentation itself impacts the received and processed message. Framing refers to the way a person’s perception of the same information can be altered simply by wording it differently, which in turn will affect their reaction and acceptance of it. For example, suppose you had just watched a long and boring movie and then your colleague asked “How long was the movie?” you’re likely to overestimate the time spent! However, if you were enjoying a comedy special and then your colleague asked, “How short was the show?” you might underestimate the total time.7
The way healthcare messages are framed has been shown to influence likelihood of people accepting/adopting or rejecting a recommended health behavior.8,9 People respond better to messages framed in a way that empowers them to avoid a threat (eg, loss of health) and enables them to maintain how they want to see themselves (ie, maintenance of their current status quo). Priming is the effect whereby a prior stimulus (eg, marketing material) will influence a person’s response to a later stimulus (eg, advice about amplification).
Of note, priming can occur even when the first stimulus is outside their conscious awareness. Expose someone to stereotypical ideas about the elderly, and it will often make them behave and feel older—even exacerbating memory problems.10-12 This begs the question, “What have we been priming all these years?”13
Unfortunately, HHPs have traditionally followed a path in direct opposition to the principles and lessons of attitudes, framing, and priming. One might argue we have unintentionally helped create the status quo (ie, “The Law of Unintended Consequences”).
The Four Questions
Alcock14 proposed four pivotal questions to understand the social norm as it relates to hearing healthcare. The response (of the patient, or of society) determines how likely they are to embrace hearing healthcare.
1) When should I have my hearing checked?
2) How can I tell if I have hearing loss?
3) Who uses hearing aids and is that relevant to me?
4) When should I use hearing aids?
To answer these questions, people depend on information they have access to at that moment in time. The obvious and prominent information exercises the greatest influence over thought processes and behaviors.15 If an answer is “common knowledge,” it has great impact.16 For example, When should I brush my teeth? [After meals or twice a day.] When should I get my vision examined? [When print is blurry and/or your “arms aren’t long enough” to read the fine print.] When should I have a physical? [Annually to maintain ideal health.]
The list goes on and on… However—and of significant importance—there are no “common knowledge” answers to the four questions posed above.
The Four Questions Answered Via the Current Social Norm
Indeed, we suspect if someone were to run a poll consisting of the four questions, the answers would approximate something like the following:
Q1. When should I have my hearing checked?
- When it’s hard to hear.
- When I need hearing aids.
- When I cannot understand anything.
- When I cannot hear spoken words.
- When I have to turn the television up really loud.
Q2. How can I tell if I have hearing loss?
- When I can no longer hear.
- When I cannot hear something I can hear now.
Q3. Who currently uses hearing aids and is that relevant to me?
- Old people, disabled people, deaf people (and it’s not relevant because I do not see myself as old, deaf, or disabled).
Q4. When should I use hearing aids?
- When I get older.
- In a few years.
- When I cannot get by without them.
Specifically, the current social norm does not offer useful (or correct) common knowledge or information—and this lack of clear guidance (to society) results in ambiguity and ambivalence; it becomes easier for a person to do nothing. Compounding this confusion is the reality that we only perceive sounds within our “hearing range.” That is, we cannot subjectively verify what we cannot hear. For many people, sounds that cannot be perceived simply cease to exist.
Shifting Our Focus: Changing the Social Norm
Traditionally, HHPs have invited people to discover they have a “condition” or a hearing impairment, while detailing how bad their condition is (ie, how flawed the person is) while pointing out the negatives (ie, “these are the sounds you can’t hear…”). HHPs subsequently offer a solution (hearing aids) that is often unexpectedly expensive and may come loaded with negative associations attached to it.
Kahneman et al17 demonstrated people are averse to the perception of loss. Others9,18-20 have shown that the threat of “having a condition” (ie, a perceived loss of health) explains why people avoid discovering they have a condition, especially if they feel powerless to minimize or prevent that loss.
Unfortunately, our traditional message/invitation is inherently negative and aversive (ie, having a hearing test or using hearing aids doesn’t minimize or prevent a hearing loss; it confirms it), and we cannot expect to change the social norm without changing the message/invitation. As Albert Einstein noted, “Insanity is doing the same thing over and over and expecting a different result.” Therefore, it may be reasonable that only 1 in 4 people with hearing loss seeks help, or that half the people who seek help choose to do nothing!
The Eight Principles for Approaching the New Social Norm
To initiate a change in the social norm, we must change the discussion from tests, loss, disability, and hearing aids, to prevention (of hearing loss and/or mishearing), evaluation/assessment, maintaining and/or improving the ability to listen and communicate maximally, and hearing technology. The hearing assessment is used to assure the patient can maximally perceive speech sounds and assures the patient can communicate maximally in work, social, and recreational situations. When we frame the discussion in terms of a loss that society can avoid, such as mishearing, we empower people to reduce that risk and maintain their status quo.
Principle 1: Focus on maximal hearing and listening. HHPs need to move away from pure-tones as the “gold standard” measure of hearing. Pure-tones are correctly used for diagnostic purposes, but do not measure listening ability or correlate at all with difficulties listening in noise. We should implement functional tests that directly record and quantify the hearing and listening ability that patients perceive, and that directly relate to their real world experience, of which the primary tool is the speech in noise (SIN) test. We also should be able to demonstrate to the patient the functional improvement through our intervention.21,22
Principle 2: Empower people through hearing technology. People want to improve or maintain their situation. Traditionally, hearing aid amplification is viewed as a negative and announces “I am flawed” because it is seen as confirmation of having a condition, rather than evidence of maintaining “maximal hearing and listening.” To be acceptable, hearing technology must allow people to maintain or increase their self-image, not decrease/deflate the same.23 People approach things that empower them and they avoid things that weaken them.24
Principle 3: Our marketing, conversations, and explanations must “mirror the perception of the patient.” When we consider hearing from the perspective of the patient with moderate or moderately severe hearing loss, we must realize they do perceive sound. As best they know, they already hear “everything,”25 but the desired sound source is not clear.
To them, that’s the problem: it’s an external one rather than internal. In a nutshell, it’s not denial or stubbornness—it’s their observation—that the sounds they want to hear are not clear! We advise making the discussion about what the patient would like to hear more of, not about what they cannot hear.
Principle 4: Situations, not shortcomings. Address the situation in which it is difficult to hear clearly, rather than requiring someone to see themselves as a person with a condition or who is impaired. The focus should be about empowering people to solve external problems rather than “spoiling their (internal) self-identity.”26
Principle 5: Ascribe positive images and attributes to hearing technology and its users. Dentists show smiling people with beautiful white teeth, not yellow crooked ones. People respond to such imagery because it models them as they want to be seen, enjoying the desired outcome. Likewise, our own marketing—from manufacturers and HHPs alike—needs to “create positive associations” in the real world by linking our own products to desired outcomes.
Principle 6: Use branding to stimulate desire for hearing technology. Brands are a powerful force in shaping consumer behavior. A good brand will extend the individual through its symbolism and associations.23,27-29
Principle 7: Normalize hearing healthcare. If hearing healthcare remains the arena of those suspected of having a condition, then those who do not see themselves as having that condition will avoid it. If the act of having your hearing checked implies you have a socially unacceptable problem, then we a priori stigmatize anyone who has their hearing tested. The role of hearing healthcare must therefore be expanded to the maintenance of “maximal hearing and listening” throughout life, and presented as normal and routine as getting a dental exam, a vision exam, and a physical.
Principle 8: Hearing healthcare must present a unified message to society. If the manufacturers, the professionals, and the state and national associations consistently repeat the same messages over and over, they supply “evidence” to the consumer to validate the same, and the message becomes “common knowledge.”30 That is, if all the “experts” say it, it must be right31 and the message becomes perceived as the social norm, which in turn influences individuals to act in accordance with that social norm.32
So then, with the above eight principles in mind, let’s address the same four questions—now reframed appropriately—as they would ideally be answered using the desired social norm so we can be clear on the direction we need to move society.
The Four Questions Answered by the Desired Social Norm and with the Eight Principles
So here are the answers to the four questions using the eight principles:
Q1. When should I have my hearing checked?
Hearing should be checked routinely throughout your lifespan, just like eyes and teeth, to maintain “maximal hearing and listening” and to avoid the consequences of mishearing in business, social, and recreational settings.
Q2. How can I tell if my hearing has changed?
Most of the time you can’t tell! Changes in hearing generally occur gradually—one hardly notices a change unless it’s a sudden onset. Indeed, if you are mishearing, it is more likely to be noticed by your family and friends before you’re aware of it.
Q3. Who currently uses hearing technology and is that relevant to me?
Frankly, it’s often impossible to tell who is wearing hearing aids because 21st century styles and technologies often render hearing technology virtually undetectable to others. In fact, many celebrities and performers use customized hearing systems to hear and listen maximally while performing as they cannot afford to miss a sound cue, direction, or discussion.
Q4. When should I use hearing technology?
Whenever the situation and/or the limitations of your hearing range compromise “maximal hearing and listening,” or increase your risk of mishearing.
Discussion, Sticky Hints, and Statistics
Sticky messages. Having established the desired responses, the hearing healthcare community must work together so our messages become “common knowledge.” The messages must be relevant, remembered, and repeatable. The best messages, quotes, and concepts are not (necessarily) yet defined. Nonetheless, here are some examples that may prove useful as a starting point:
1) Eyes checked. Teeth checked. Hearing checked.
2) Be wise, check hearing like eyes!
3) If you ask to repeat, check your hearing’s complete.
4) Others will tell if I’m not hearing well.
5) Better to know before problems show.
6) Hear to stay, not fade away.
Social Proof. Ultimately, social norms are about the perception of most people in society. If people assume hearing healthcare is for the minority, those people who are uncertain (about the relevance of hearing healthcare) will follow the majority and do nothing. Cialdini32 refers to this as “social proof.”
Therefore, it’s generally not wise to tell the public “10% of the people in the USA have hearing loss” and “only 1 in 4 seek help for their hearing difficulty.” Clearly, the other side of that coin, and the message the public is getting, is 90% of all people don’t have hearing loss, and even if they do, 75% don’t seek help for their hearing difficulty (so you probably don’t need to either!).
Maximal hearing and listening. When we focus on “maximal hearing and listening,” the message is relevant to the majority and about maintaining (or improving) your place among that majority. When we combine this with consistent messages and marketing to increase people’s awareness that hearing healthcare is commonplace, we create a self-fulfilling prophecy.
Hearing healthcare has a truly remarkable and transformative product that already has many millions of satisfied users. What it suffers from is an image problem. It’s time for us to change that. The principles offered in this article are the first step in accomplishing this.
References
1. Kochkin S, Beck DL. 35 million people in the USA with hearing loss. Presentation at: Galloway, NJ; spring 2013.
2. Amlani A, Taylor B. Three known factors that impede hearing aid adoption rates. Hearing Review. 2012;19(5):28-37. Available at: https://hearingreview.com/2012/05/three-known-factors-that-impede-hearing-aid-adoption-rates
3. Kochkin S. MarkeTrak VIII: 25 year trends in the hearing health market. Hearing Review. 2009;16(11):12-31. Available at: https://hearingreview.com/2009/10/marketrak-viii-25-year-trends-in-the-hearing-health-market
4. Petty RE, Cacioppo JT. Source factors and the elaboration likelihood model of persuasion. In: Kinnear TC, ed. NA—Advances in Consumer Research. Vol 11. Provo, Utah: Association for Consumer Research; 1984:668-672.
5. Petty RE, Cacioppo JT. The Elaboration Likelihood Model of persuasion. In: Berkowitz L, ed. Advances in Experimental Social Psychology. Vol 19. New York: Academic Press; 1986:123-205.
6. Chaiken S, Maheswaran D. Heuristic processing can bias systematic processing: effects of source credibility, argument ambiguity, and task importance on attitude judgment. J Pers Soc Psychol. 1994;66:460-473.
7. Harris R. Answering questions containing marked and unmarked adjectives and adverbs. J Exp Psychol. 1973;97:399-401.
8. Levin IP, Schneider SL, Gaeth GJ. All frames are not created equal: a typology and critical analysis of framing effects. Organizational Behavior and Human Decision Processes. 1998;76:149-188.
9. Rothman AJ, Salovey P. Shaping perceptions to motivate healthy behaviour: the role of message framing. Psychol Bull. 1997;121:3-19.
10. Bargh JA, Chen M, Burrows L. Automaticity of social behavior: direct effects of trait construct and stereotype activation on action. J Pers Soc Psychol. 1996;71(2):230-44.
11. Barber SJ, Mather M. Stereotype threat can both enhance and impair older adults’ memory. Psychol Sci. 2013;24(12):2522-2529.
12. British Psychological Society (BPS). You are as old as you feel. ScienceDaily online. 2013, April 9. Available at: www.sciencedaily.com/releases/2013/04/130409091219.htm
13. Bargh JA. What have we been priming all these years? On the development, mechanisms, and ecology of nonconscious social behavior. Eur J Social Psychol. 2006;36(2):147-168.
14. Alcock CJ. The 4 Questions. 2013. Available at: www.audira.info
15. Fishbein M, Ajzen I. Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. Reading, Mass: Addison-Wesley; 1975:Chapter 6.
16. Vanderschraaf P, Sillari G. “Common Knowledge” In: Zalta EN, ed. The Stanford Encyclopedia of Philosophy [Fall 2013 Edition].
17. Kahneman D, Knetsch JL, Thaler RH. Anomalies: the endowment effect, loss aversion, and status quo bias. Journal of Economic Perspectives. 1991;5(1):193-206.
18. Rothman AJ, Bartels RD, Wlaschin J, Salovey P. The strategic use of gain- and loss-framed messages to promote healthy behavior: how theory can inform practice. Journal of Communications. 2006;56:S202–S220.
19. Dawson E, Savitsky K, Dunning D. “Don’t tell me, I don’t want to know”: understanding people’s reluctance to obtain medical diagnostic information. J Appl Soc Psychol. 2006;36(3):751-768.
20. Norman P, Boer H, Seydel ER. Protection motivation theory. In: Conner M, Norman P, eds. Predicting Health Behaviour: Research and Practice with Social Cognition Models. London: Open University Press; 2005:81-126.
21. Beck DL, Nilsson M. Speech-in-noise testing—a pragmatic addendum to hearing aid fittings. Hearing Review. 2013;20(5):24-26. Available at: https://hearingreview.com/2013/05/speech-in-noise-testing-a-pragmatic-addendum-to-hearing-aid-fittings-2
22. Beck DL, Repovsch JL. Observations on speech, speech in noise, and embedded tests. Hearing Review. 2013;20(8):22-24. Available at: https://hearingreview.com/2013/07/observations-on-speech-speech-in-noise-and-embedded-tests
23. Zinkhan GM, Hong JW. Self concept and advertising effectiveness: a conceptual model of congruency conspicuousness, and response mode. In: Holman RH, Solomon MR, eds. Advances in Consumer Research. Vol 18. Provo, Utah: Association for Consumer Research; 1991:348-354.
24. Keltner D, Gruenfeld DH, Anderson C. Power, approach, and inhibition. Psychol Rev. 2003;110:265-284.
25. Sharov AA. Umwelt theory and pragmatism. Semiotica. 2001;Vol 2001(134):211-228.
26. Goffman E. Stigma: Notes on the Management of Spoiled Identity. New York: Simon & Schuster; 1963:Chapter 2.
27. Shavitt S, Nelson MR. The social identity function in persuasion: communicated meanings of product preferences. In: Maio GR, Olson JM, eds. Why We Evaluate: Functions of Attitudes. Mahwah, NJ: Erlbaum; 2000:37-57.
28. Elliott R, Wattanasuwan K. Brands as symbolic resources for the construction of identity. International Journal of Advertising. 1998;17:131-144.
29. Escalas JE, Bettman JR. Self?construal, reference groups, and brand meaning. Journal of Consumer Research. 2005;32(3):378-389.
30. Hawkins SA, Hoch SJ. Low-involvement learning: memory without evaluation. Journal of Consumer Research. 1992;19(2):212-225.
31. Cialdini RB, Goldstein NJ. Social influence: compliance and conformity. Ann Rev Psychol. 2004;55:591–621.
32. Cialdini RB. Influence: Science and Practice. 5th ed. Boston: Pearson: 2008;Chapter 4.
Other recommended reading:
Amlani AM. Will federal subsidies increase the US hearing aid market penetration rate? Audiology Today. 2010;22(3):40-46.
Chaiken S. Heuristic versus systematic information processing and the use of source versus message cues in persuasion. J Pers Soc Psychol. 1980;39(5):752-766.
Ditto PH, Munro GD, Apanovitch AM, Scepansky JA, Lockhart LK. Spontaneous skepticism: the interplay of motivation and expectation in responses to favorable and unfavorable medical diagnoses. Pers Soc Psychol Bull. 2003;29(9):1120-1132.
Fiske ST, Taylor SE. Social Cognition: From Brains to Culture. 2nd ed. Los Angeles: Sage; 2013:Chapter 5,136-144.
Keenan J. Framing a Sales Call to Overcome Your Prospects’ Objections. 2013. Available at: http://blog.hubspot.com/sales/framing-a-sales-call-to-overcome-prospects-objections
Samuelson W. Zeckhauser R. Status quo bias in decision making. Journal of Risk and Uncertainty. 1988;1:7-59.
Shavitt S. The role of attitude objects in attitude functions. J Exp Soc Psychol. 1990;26:124-148.
Swann WB Jr. Self-verification: bringing social reality into harmony with the self. In: Suls JM, Greenwald AG, eds. Social Psychology Perspectives. Vol 2. Hillsdale, NJ: Erlbaum; 1983:33-66.
Douglas L. Beck, AuD, is the director of professional relations at Oticon Inc, Somerset, NJ. Curtis J. Alcock is founder of Audira »Think Tank for Hearing (www.audira.org.uk) and has worked as a hearing care professional in the United Kingdom.
Correspondence can be addressed to Dr Beck at: [email protected]
Original citation for this article: Beck DL, Alcock CJ. Right product; Wrong message. Hearing Review. 2014;21(4): 16-21.