Research | November 2020 Hearing Review
Research shows how to assist GPs with early detection and timely treatment choices
By Rebecca Bennett, PhD, and Caitlin Barr, PhD
For people with hearing loss, the family physician (aka, general practitioner or primary care doctor) can be key to early detection and guiding appropriate and timely treatment choices. But how can hearing care professionals work with family physicians to get hearing loss front and center on their agenda?
The family physician or general practitioner (GP) is often the first point of contact for people seeking advice or referral about their hearing.1 However, screening for hearing loss and providing timely and appropriate referrals are not routine in primary care.1,2 Up to 85% of older patients receive no spontaneous advice from their family physician about their hearing. Even when these patients specifically raise concerns about their hearing these can be dismissed.1,3 Family physicians may be aware of their older patients’ risk of hearing loss but are uncertain how to arrange early intervention.4,5 They may have doubts about hearing aid effectiveness and whether their older patients see their hearing loss as a priority. Therefore, although family physicians are well placed to support patients in their management of age-related hearing loss, they may not be identifying hearing loss, actively encouraging help-seeking, or referring patients to hearing specialist services.
The Family Physician’s Role in Managing Age-related Hearing Loss
We recently conducted a program of research exploring how the family physician manages age-related hearing loss. This included a systematic review6 of the literature, and a qualitative study with key stakeholders. Our review identified 49 peer-reviewed journal articles about how hearing loss is managed in primary care across three themes:
- Detection and diagnosis of hearing loss;
- Management and referral for hearing loss, and
- Knowledge of and attitudes toward hearing loss.
Detection and diagnosis of hearing loss. Family physicians have quick, easy, and sensitive methods available to detect and diagnose hearing loss.6 However, hearing screening is often underutilized and/or performed only when requested by the patient.3,5,7
Routine hearing screening programs targeting older adults will raise detection rates and subsequently increase the number of patients receiving hearing loss intervention.6 Some family physician clinics have hearing screening equipment available but their staff lack the skills to effectively use it. The staff may also not know how to effectively triage the clients following a diagnosis of the hearing loss. Audiologists and hearing care professionals (HCPs) should be able to support their local family physicians and their staff by providing appropriate training and support.
Management and referral for hearing loss. Patient outcomes improve when the family physician manages and refers for hearing loss.8 However, hearing loss referral by family physicians remains low.1 The physician may be uncertain about where to refer their patients,9 have concerns regarding HCPs’ qualifications,5 and hold negative perceptions about how older patients prioritize hearing.4
Methods to improve family physicians’ referral rates for hearing care services can include standard referral letters, family physician waiting room wall posters and leaflets, family physician training on the impacts of hearing loss and the benefits of hearing aids, and supplying the practice with patient educational brochures.6 Audiologists have a potential role in providing information and training to family physicians about referral processes, hearing loss management options, and client outcomes from audiological rehabilitation.
Knowledge of and attitudes toward hearing loss. Family physicians are highly knowledgeable about their older patients’ susceptibility to hearing loss and impact on their quality of life. However, they are less positive about their role in hearing loss management as many are unsure about how effective and usable hearing aids could be.4,5
Our review concluded that information and training appear to be key actions to improving family physicians’ screening, management, and referral of patients with hearing loss. HCPs can play a role by partnering with local family physicians to raise awareness, improve knowledge, and strengthen referral partnerships. Potentially useful methods to achieve these include:
1) Educational brochures designed for the family physician setting,3
2) Structured referral forms and providing family physicians with demonstration hearing aids to support discussions with patients,10 and
3) Family physician training.11
Factors in Detecting, Discussing, and Recommending Action Regarding Hearing Loss within Family Physicians
In addition to our review, we used concept mapping techniques to gain an in-depth understanding of the barriers and facilitators to detecting, discussing, and recommending action regarding hearing loss within family physician consultations.12 We gathered the perspectives of family physicians (n=8), adults with hearing loss (n=22), and professionals working with family physicians (such as practice managers or practice nurses (n=5) in Australia. Participants generated statements in response to the prompt “In my opinion, the role and responsibility of family physicians in managing age-related hearing loss is…” Approximately 2 weeks later, via an online portal, participants then grouped the statements to identify key themes.
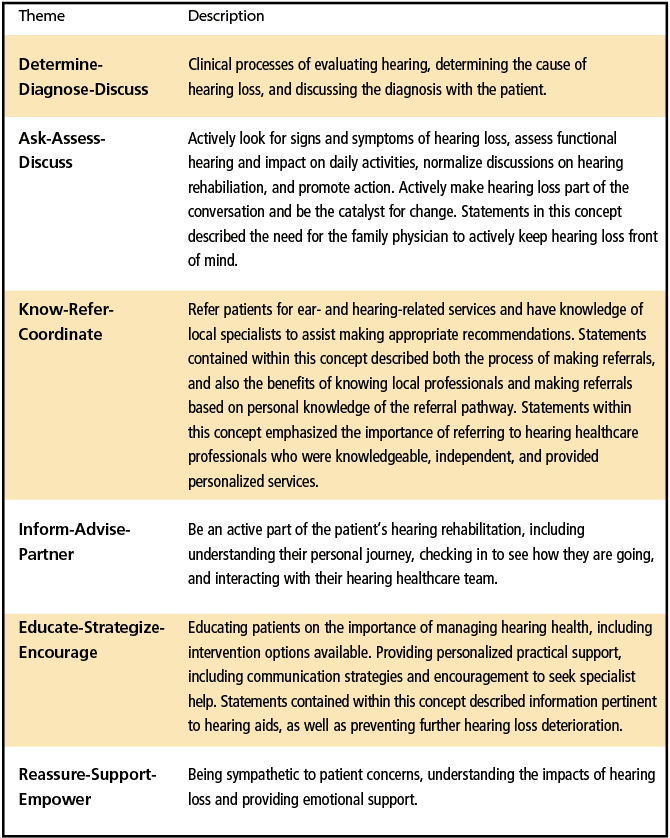
Participants identified 98 individual statements across six concepts describing the role of the family physician in managing age-related hearing loss (Table 1).12 These included both biomedical (such as detection, diagnosis, treatment and referral) and person-centered (such as listening, supporting, motivating, and reassuring) approaches to patient care.
Participants described the role of the family physician in early detection of hearing loss. They expected family physicians to detect the subtle signs of hearing loss, raise their concerns, normalize conversations about hearing loss, and monitor patients as they age.12
It is important to keep in mind however, that family physicians are responsible for detecting the widest range of conditions of any medical speciality.13 They are time poor and need to prioritize what they perceive as the most pressing health conditions. Furthermore, hearing loss may not be visible to the family physician, and patients are unlikely to spontaneously raise their hearing concerns. It is no wonder that family physicians do not routinely detect hearing loss in their patients.
The importance of multidisciplinary care and the family physician’s role in coordinating this was particularly highlighted through the Know–Refer–Coordinate concept (see Table 1). The statements contained within this theme described not only the process of referral to audiology services, but the importance of the family physician having knowledge of who they are referring to, and to refer to reputable hearing services. Improving relationships between family physicians and allied health practitioners was identified as an effective strategy to address barriers to successful referrals.
Requesting and providing feedback (monitoring quality) and delivering training and/or resources were also considered effective strategies to address barriers to referral. Family physicians may not necessarily have the time to build relationships with potential referrers, thus there may be a role for HCPs to play in reaching out to local family physicians, developing professional networks, and building referral partnerships.
Our research has identified a number of ways in which HCPs can assist family physicians with early detection, and guiding appropriate and timely treatment choices for age-related hearing loss. These include:
- Improving hearing loss detection rates through offering local family physicians and their staff appropriate training and support relating to hearing loss detection, including how to use the audiometer, interpret results, and triage appropriately.
- Helping family physicians keep hearing loss front of mind by providing them with visual cues, such as waiting room posters, brochures, screening tools, visual reminders (such as a model of the ear for display and demonstration on the desk), and raising awareness of hearing in professional magazines.
- Building a professional relationship with local family physicians to promote bidirectional referrals, and keeping each other informed on what is going on with the patient.
- Educating local family physicians on the range of audiological services available, and the success of these services.
In light of this research, it appears that the more proactive audiologists are in engaging with local family physicians, practice managers and nurses, the better outcomes patients will receive.

Correspondence can be addressed to Dr Bennett at: [email protected].
Original citation for this article: Bennett B, Barr C. How do family physicians manage age-related hearing loss? Hearing Review. 2020;27(11):14-16.
References
- Schneider JM, Gopinath B, McMahon CM, et al. Role of general practitioners in managing age-related hearing loss. Med J Austral. 2010;192(1):20-23.
- Johnson CE, Danhauer JL, Koch LL, Celani KE, Lopez IP, Williams VA. Hearing and balance screening and referrals for Medicare patients: A national survey of primary care physicians. J Am Acad Audiol. 2008;19:171-190.
- Wallhagen MI, Pettengill E. Hearing impairment: Significant but underassessed in primary care settings. J Gerontol Nursing. 2008;34(2):36-42.
- Gilliver M, Hickson L. Medical practitioners’ attitudes to hearing rehabilitation for older adults. Int J Audiol. 2011;50(12):850-856.
- Danhauer JL, Celani KE, Johnson CE. Use of a hearing and balance screening survey with local primary care physicians. Am J Audiol. 2008;17(1):3-13.
- Bennett RJ, Conway N, Fletcher S, Barr C. The role of the general practitioner in managing age-related hearing loss: A scoping review. Am J Audiol. 2020;29(2):265-289.
- Cooper GS, Goodwin MA, Stange KC. The delivery of preventive services for patient symptoms. Am J Prevent Med. 2001;21(3):177-181.
- Hands S. Hearing loss in over-65s: Is routine questionnaire screening worthwhile? J Laryngol Otol. 2000;114(9): 661-666.
- Cohen SM, Labadie RF, Haynes DS. Primary care approach to hearing loss: The hidden disability. ENT Jour. 2005;84(1):26-44.
- Kapteyn TS, Wijkel D, Hackenitz E. The effects of involvement of the general practitioner and guidance of the hearing impaired on hearing-aid use. Brit J Audiol. 1997;31(6):399-407.
- Kochkin S. BHI physician program found to increase use of hearing healthcare. Hear Jour. 2004;57(8): 27-29.
- Bennett RJ, Fletcher S, Conway N, Barr C. The role of the general practitioner in managing age-related hearing loss: Perspectives of general practitioners, patients and practice staff. BMC Family Practice. 2020;21(87).
- Cooke G, Valenti L. Glasziou P, Britt H. RACGP: Common general practice presentations and publication frequency. Austral Fam Phys. 2013;42(1):65.





