Hearing Testing | September 2018 Hearing Review
The foundations of today’s pure-tone audiometry and the arduous road to automation
Three methods of conducting pure-tone audiometry have dominated how we assess hearing for almost 70 years. Here is a historical look at the evolution of the audiometric technique, how automation and automated adaptive techniques continue to evolve, and a perspective on what might prompt significant changes for the future.
For almost 100 years the pure-tone audiogram has been central to audiological evaluation, usually the prime metric for establishing the nature and extent of hearing loss. This article traces the evolution of the procedures used to define audiometric thresholds as they have changed—and resisted change—over time. We begin with a short historical review of the classical psychophysical methods for estimating thresholds.
The Psychophysical Methods

Figure 1. Gustav Fechner was a pioneer of psychophysics and developed the three classical psychophysical menthods: The Method of Limits, the Method of Adjustment, and the Method of Constant Stimuli.
Early audiology borrowed heavily from the psychological research of Gustav Theodor Fechner (1801-1887), a German philosopher and scientist who pioneered the study of what we now call psychophysics (Figure 1).1 In order to understand the relation between physical stimuli and human responses, he asked what is the minimal stimulus strength, or “threshold,” below which there is no awareness of the stimulus. To this end he developed three methods of measurement, now called the three classical psychophysical methods:
- The Method of Limits;
- The Method of Adjustment, and
- The Method of Constant Stimuli.
Both the Method of Limits and the Method of Adjustment have figured prominently in the development of pure-tone audiometric testing. (The Method of Constant Stimuli was never in the running because you must construct an entire input-versus-output function before you can estimate a single threshold.)
In the Method of Limits, the strength of the stimulus is reduced until there is no response (a descending run), then increased from below this point until a response first appears (an ascending run). This sequence of descending and ascending runs is repeated three or more times. Threshold is defined as the midpoint between the average of descending runs and the average of ascending runs. Typically, the average of descending runs is slightly better (less stimulus strength), than the average of ascending runs.
In the Method of Adjustment, the listener is given control of the intensity level of the stimulus and instructed to adjust it to the level at which the stimulus is just barely discernable. Successive trials are averaged to define the threshold response.
In the following sections, we trace the development of audiometric techniques based on the Method of Limits, the Method of Adjustment, and modern Adaptive techniques for estimating pure-tone thresholds.
The First Audiologist
Modern clinical audiometry began in the 1920s with the seminal publications of Cordia C. Bunch.2,3 As a graduate student in the Department of Psychology at the University of Iowa in the years immediately following World War I, Bunch would have been familiar with the work of Fechner and the three classical psychophysical methods. In his 1943 book, Clinical Audiometry,4 Bunch gave a fairly detailed description of his technique, a straightforward application of the classical Method of Limits. Bunch began by presenting a continuous tone at a level easily heard. Patients pressed a button to indicate that they heard it. He immediately turned the sound off, decreased the intensity, and turned on the continuous sound again. In this fashion he decreased the intensity level until the listener stopped responding. He then dropped well below this level, turned on the continuous tone again, and repeated the sequences in an ascending direction, until the patient responded. This procedure was repeated three or four times. Threshold was defined as the level midway between the average of the descending and the average of the ascending runs. This was the essence of Bunch’s technique: a clear application of Fechner’s Method of Limits.
During the 1930s, other clinicians followed this technique in the process of gathering their clinical audiograms. Some suggested that thresholds seemed more stable if the tone was turned on in short bursts against a background of silence, rather than continuous stimulation with only short breaks of silence as the level was changed. Partly, this concern arose because many noted that subjects adapted to the loudness of high-frequency tones (especially 4000 and 8000 Hz) quickly if the tone was presented for any length of time, particularly if there was hearing loss at these high frequencies. Many clinicians also observed that, when using 5-dB steps, there was little difference between the threshold levels revealed by descending versus ascending runs. Some also noted that the threshold level defined by the ascending run seemed more stable.
These various observations prompted in 1944 a paper of major historical significance by Walter Hughson and Harold Westlake.5 Hughson and Westlake successfully codified the consensus among many working clinicians of the time about how to measure audiometric thresholds. It was based on Bunch’s early description but incorporated the important difference that short tone-bursts should be heard against a background of silence rather than long continuous tones be heard, separated only briefly by short intervals of silence as the level was changed. These two procedures are contrasted in Figure 2. It further recommended that threshold be defined solely by an ascending series of tonal presentations.

Figure 2. Contrasting Bunch’s original technique with the subsequent Hughson-Westlake technique. In Bunch’s method, the test tone was on almost continuously, being interrupted only when the intensity level was changed. By contrast, in the Hughson-Westlake method, short tone bursts are separated by longer periods of silence as the intensity level is changed. Note also that Bunch approached threshold from both directions while Hughson-Westlake relies heavily only on an ascending series.
Thus, the Hughson-Westlake recommendations became known as the “ascending method.” The threshold was usually defined as the lowest level at which there had been a response at 2 out of 3 ascending runs. Finally, as a result of on-effect and adaptation studies during the 1950s, Carhart and Jerger6 fleshed out the details of the Hughson-Westlake method that were not elaborated in the original article, discussed the psychoacoustic foundations of clinical threshold testing, compared ascending and descending protocols, discussed the 5-dB step size that is now in nearly universal use, and established a sound scientific basis for pure-tone threshold testing. Over the next half century, this method for plotting clinical audiograms remained essentially unchanged.
Breaking Out of the Mold: Automation
Wayne Rudmose7 was an acoustical engineer at Southern Methodist University who pioneered the fabrication and testing of some of the earliest versions of automated audiometers. In the early years of the 1960s, he wrote:
Seldom does an engineer take point-by-point data by hand unless special, specific problems arise. Thus, it appears only natural that those features of audiometry which can be automated will be, and the audiologist will find himself fully occupied with the task of analyzing and interpreting the data. The routine work can be done by the machine. [p 31] 7
Some 42 years later, in a paper entitled “Automated Audiometry: Progress or Pariah?” Robert Margolis made the same point:
Doctoral level healthcare providers should not spend their time performing routine tasks that, for most of our patients, are amenable to automation.8
The decades of the 1950s and 1960s saw a flurry of surprisingly sophisticated attempts at automation, driven primarily by the need to screen for hearing loss in large groups of industrial workers and in recruits for the various military services. In his chapter, “Automatic Audiometry,” Rudmose7 reviewed the various screening systems designed for these essentially group applications by Ward, Webster, Glorig & Wilke, Reger & Voots, Brogan, Weiss, High & Glorig, and Rudmose himself. Eventually some of these systems for testing groups morphed into devices suitable for testing individuals. The Rudmose ARJ-4 began as a group screener, using a tracking method at individual discrete frequencies. It could also be used as an individual test unit: the ARJ-4 automatic self-recording audiometer (Figure 3).

Figure 3. The Rudmose ARJ series of audiometers offered automated intensity, frequency, and data recording.
Perhaps the largest single study comparing conventional with automated audiometry was carried out by Aram Glorig at the 1955 Wisconsin State Fair.7 More than 400 Fair attendees were tested both with a conventional audiometer and with the Rudmose ARJ-4 automatic audiometer. Mean differences between the manual and the automated results across six frequencies and two ears ranged from 0.1 dB to 7.8 dB (both differences at 6 kHz); all other mean differences were within that range.
An Exercise in Frustration
The calls to action by Rudmose and Margolis reminded me of my first attempt, in 1972, to introduce a modicum of automation into our hearing clinic at The Methodist Hospital in Houston. It seemed to me that pressing a lever to turn on each tone for an uncontrolled duration at uncontrolled inter-tone intervals could surely benefit from automation. I modified an audiometer in which the Hughson-Westlake technique was partially automated. An electronic switch, triggered by an electronic timer, created a continuous train of tones. The duration of each tone was exactly 500 milliseconds, and the inter-tone interval varied randomly between 4 seconds and 6 seconds. Between tones the operator could vary the hearing-loss dial according to any sequence deemed appropriate and could change the frequency at will.
It was a very minimal approach to automation, but I thought that at least tone duration and inter-tone silent intervals were controlled, and the need for lever pushing to initiate each short tone was eliminated. I assigned one of our audiologists to try out the new audiometer and tell me what he thought. “Bob,” I said, “you are going to have the privilege of ushering in a new era in audiology. You will no longer need to push a lever to turn on each tone. That will be done automatically. The duration of each tone presentation will be precisely controlled, and the interval between tone bursts will be randomized over a defined range of durations. All you have to do is change the level before each tone is presented. I want you to work with it for awhile and then tell me what you think.”
After several days he reported that he wanted his old audiometer back. Somewhat surprised, I asked him why he didn’t like the new device. He was reluctant to answer at first but finally volunteered that in school he had learned a different way of doing it; he was uncomfortable with the new device because this was not how he had learned to do audiograms. In particular, he stressed that the timing of when the tone was turned on or off should be under his own immediate control. Otherwise it just didn’t seem right to him. After mulling that for a long time I concluded that progress with automation would drag until initial educational training in audiometry itself featured some degree of automation. Until that happened, I thought, progress with any form of automation would be painfully slow.
That was 48 years ago, and I am sorry to say that my foreboding was warranted.
Recent Efforts to Automate Audiometry
Recent approaches to automate pure-tone audiometry fall into three general categories:
- Automation of the Method of Limits (Hughson-Westlake Technique);
- Automation of the Method of Adjustment (Békésy-type Tracking Audiogram), and
- Automation of Adaptive Methods.
1) Automated Method of Limits
Many efforts to automate a system to gather pure-tone audiograms have, not unreasonably, begun with the premise that powerful technology should be employed to automate the Hughson-Westlake technique that every audiologist knows and uses. Over the past four decades there have been a number of attempts to automate the simple rules governing Hughson-Westlake threshold searches.
In a meta-analysis of the validity of automated threshold audiometry based on the Method of Limits, Mahomed et al9 reviewed 13 studies in which automation was achieved based on the Hughson-Westlake protocol. In each study the difference between conventional and automated air conduction thresholds was not statistically significant. A similar result was reported by Swanepoel et al.10 Based on tests of both normal-hearing listeners and actual patients, they concluded that “Automated audiometry provides reliable, accurate, and time-efficient hearing assessments for normal-hearing and hearing-impaired adults” [p 557].
2) Automated Method of Adjustment
Perhaps, reasoned some investigators, rather than perseverating on automating the Hughson-Westlake protocol, it might be wiser to ask whether Hughson-Westlake is the best procedure to automate. The renowned Hungarian scientist, Georg von Békésy, approached the problem from a different direction. During World War II, at the Karolinska Institute in Stockholm, he designed and built a fully automated audiometer.11 A pair of motors drove both the intensity level and the frequency of the test tone at constant speed. Patients tracked their own thresholds by means of a motor reversal switch, pressing a button when the test tone was no longer audible, then releasing the button when the tone was just audible, to produce a self-recorded audiogram—eventually called a “Békésy audiogram.” It was essentially an automation of Fechner’s classical Method of Adjustment and has come to be called “Tracking.” All of this goes back more than 50 years.
Did the Békésy audiogram actually work in the audiology clinic? I can report two known successful applications. One was reported by Margolis in the article referenced above:
In 1984…I visited the private practice of…Alan Feldman…During our visit I observed Dr. Feldman testing a patient with the automated pure-tone Békésy tracking method. While the audiogram was being recorded, he attended to other things…That was the first and only time I saw Békésy audiometry used for routine threshold audiometry in a clinical setting.8
The second successful clinical application of self-tracking audiometry was carried out by our team at the Baylor College of Medicine in Houston in the late 1960s. We set up an audiology clinic in The Methodist Hospital in the Texas Medical Center, designed around a Grason-Stadler E-800, Békésy-type audiometer. While at Northwestern University in the late 1950s, we had successfully tested more than 400 patients with a Grason-Stadler E-800 audiometer12; however, that was in a research rather than a clinical setting. Later, in our hospital clinic in Houston, we were curious to see how it would work out as the primary source of clinical audiograms. We successfully tested more than 300 patients. Overall, we judged our experiment with automated Békésy audiometry to be quite successful.
In their comprehensive review and meta-analysis of the validity of automated audiometry cited earlier, Mahomed et al9 also identified 16 studies involving a comparison between conventional (Hughson-Westlake) and an automated method of adjustment technique. Again, there were no statistically significant differences between conventional and automated air-conduction thresholds.
3) Automated Adaptive Methods
While most clinicians continued to employ conventional manually-operated audiometers, psychoacousticians were busy developing more efficient methods for quickly identifying thresholds.13,14 Called “adaptive psychophysical methods,” they emphasize stimulus sequences that quickly establish an estimated threshold, then oscillate about this point until a valid threshold halfway between “heard” and “not heard” has been established. One might think of this as a basically speeded up, more efficient, variation on the classical Method of Limits. Rather than counting only ascending directions, it can accommodate any of several possible up-down rules such as:
- “heard”—go down; “not heard”—go up,
- “heard, heard”—go down; “not heard”—go up, or,
- “heard”—go down; “not heard, not heard”—go up.
Even more elaborate variations can be imagined and implemented. New techniques like these can be automated to produce pure-tone audiograms equivalent to those produced by human operators who follow a conventional Hughson-Westlake strategy.9,10,15-17
Perhaps the most thoroughly evaluated of such systems to date is AMTAS (Automated Method for Testing Auditory Sensitivity) developed by Robert Margolis and his colleagues.15-17 It finds the threshold at each test frequency by an adaptively implemented Method of Limits. An AMTAS-based system is now commercially available from Grason-Stadler Inc (GSI), but still awaits widespread usage.
Concluding Thoughts
Based on my experiences 50 years ago, my heart still belongs to the Békésy version of the Method of Adjustment. It kept the listener engaged in the task from start to finish, and yielded valid results. I still like its simplicity and versatility. Yet, my head says that if my colleagues prefer an automated system based on the Method of Limits, so be it. The most important issue is to catch up with the rest of the automated world.
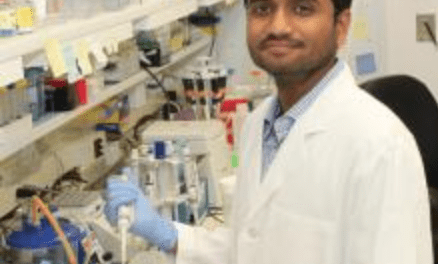
In spite of the many examples of successful automated systems summarized above, I suspect that there will be little further progress in the actual clinical use of automated audiometry of any variety until clinicians become part of the solution. It goes back to their initial educational experience. If the only procedure they learn as students is the manual Hughson-Westlake method on a conventional audiometer, it is unlikely that they will be easily diverted from that familiar path, sophisticated technology notwithstanding. PhD and AuD students—in addition to practicing clinicians—need to understand that automated audiometry can be carried out by less credentialed personnel, resulting in time and cost savings in a clinical setting. It is apparent this testing is moving into the digital/consumer realm (Figure 4).

Figure 4. Screenshot from a recent Apple WWDC18 online video18 in which Apple software engineer Srinath Tupil Muralidharan explained how the company’s ResearchKit for software developers uses the Hughson-Westlake pure-tone threshold method, as well as an assessment of the noise level in the test environment.
In the final analysis, appeals to the bottom line may be more successful than appeals to reason. Additionally, as advocated in my July 2018 Hearing Review article,19 which was part of a broader series on audiology and neuroscience, the widespread adoption of more sophisticated testing methods and technologies that are based on solid science should lead to greater efficiency in the clinic and better rehabilitation strategies and outcomes for at least some (if not most) patients who ultimately seek our professional guidance.
Acknowledgment
I am grateful to Richard Tyler for suggesting this article, to Robert Margolis for his many contributions to automated audiometry, and to Susan Jerger for expert editing of this article.
Correspondence can be addressed to HR or Dr Jerger at: [email protected]
Original citation for this article: Jerger J. The evolution of the audiometric pure-tone technique. Hearing Review. 2018;25(9):12-18.
References
-
Fechner GT. Elemente der Psychophysik, Vol 1. Leipzig, Germany: Breitkopf & Härtel;1860.
-
Bunch CC. Measurement of auditory acuity throughout the tonal range. Psychol Monogr.1922;31(1):45-82.
-
Bunch CC. New procedure in tests of auditory acuity. J Opt Soc Amer. 1923;7(12):1161-1166.
-
Bunch CC. Clinical Audiometry. St Louis, MO: The C.V. Mosby Company;1943.
-
Hughson W, Westlake HD. Manual for program outline for rehabilitation of aural casualties both military and civilian. Trans Am Acad Ophthal Otolaryng. 1944;48 [Suppl]:1-15.
-
Carhart R, Jerger JF. Preferred method for clinical determination of pure-tone thresholds. J Speech Hear Dis. 1959;24(4):330-345.
-
Rudmose W. Automatic audiometry. In Jerger J, ed. Modern Developments in Audiology. 1st ed. New York,NY: Academic Press; 1963.
-
Margolis RH. Automatic audiometry: Progress or pariah? January 17, 2005. Available at: https://bit.ly/2Kzqofv
-
Mahomed F, Swanepoel DW, Eikelboom RH, Soer M. Validity of automated threshold audiometry: A systematic review and meta-analysis. Ear Hear. 2013;34(6):745-752.
-
Swanepoel DW, Mngemane S, Molemong S, Mkwanazi H, Tutshini S. Hearing assessment-reliability, accuracy, and efficiency of automated audiometry. Telemedicine and e-Health. 2010;16(5).
-
Békésy GV. A new audiometer. Acta Oto-laryng. 1947;35(5-6):411-422.
-
Jerger J. Békésy audiometry in analysis of auditory disorders. J Speech Hear Res. 1960;3(3):275-287.
-
Levitt H. Transformed up-down methods in psychoacoustics. J Acoust Soc Amer. 1971;49(2B):467-477.
-
Leek MR. Adaptive procedures in psychophysical research. Perception and Psychophysics. 2001;63(8):1279-1292.
-
Margolis RH, Glasberg BR, Creeke S, Moore BCJ. AMTAS: Automated method for testing auditory sensitivity: Validation studies. Int J Audiol. 2010;49(3):185-194.
-
Margolis RH, Frisina R, Walton JP. AMTAS: Automated method for testing auditory sensitivity: II. Air conduction audiograms in children and adults. Int J Audiol.2011;50(7):434-439.
-
Margolis RH, Moore BCJ. AMTAS: Automated method for testing auditory sensitivity: III. Sensorineural hearing loss and air-bone gaps. Int J Audiol.2011;50(7):440-447.
-
Muralidharan ST, Blanco G, Yadav A. Advances in research and care framewords. Presentation at: Apple WWDC18 [Session 205]; June, 2018; San Jose, CA. Relevant clip found at 10:40.
-
Jerger J. Clinical speech audiometry in the age of the AERP. Hearing Review. 2018;25(7):14-19.





I’m somewhat surprised to learn that more recent automated adaptive threshold estimation techniques, developed by psychophysics researchers, are apparently not in wider use by Audiologists. These methods are very sophisticated and entirely automated. One highly used method is QUEST (Watson & Pelli, 1983), which uses Bayesian statistics to more rapidly and efficiently estimate perceptual thresholds for hearing, vision, touch, taste or smell, and for any sort of percept within a modality (e.g., in the auditory modality: pure tones, speech, real-world sounds, sound locations, etc.). Another is SIAM (Kaernbach, 1990), which uses Signal Detection Theory to differentially weight true positives, false positives, true negatives, and false negatives. This includes catch trials, in which no stimulus is presented. This allows for the possibility that the person being tested sometimes makes false negative responses, which are systematically accounted for by the threshold estimation procedure.
Watson, A. B., & Pelli, D. G. (1983). QUEST: A Bayesian adaptive psychometric method. Perception & psychophysics, 33(2), 113-120.
Kaernbach, C. (1990). A single‐interval adjustment‐matrix (SIAM) procedure for unbiased adaptive testing. The Journal of the Acoustical Society of America, 88(6), 2645-2655.
Its sure bin a long journey in threshold measurements. Thanks for the memories!
Thank you Dr. Jerger for reminding us of this history and much more. After nearly 40 years of monitoring who knows how many million pure tone beeps, I too yearn for automation, but two additional considerations prevail. First, automation can work well with an individual diligently volunteering his best hearing acuity, but experience reveals a world full of patients who have other agendas. To my knowledge, no better meter exists for evaluating the validity of a hearing test than the hairs on the back of one’s neck! Second, especially for those in private practice, the audiologist’s interaction with the patient during testing yields tremendously useful insight into the subtleties of that individual’s hearing deficit and other cognitive capabilities that help to shape the rehab plan. Nothing yet seems to beat the person-to-person hearing evaluation.