Research | February 2015 Hearing Review
Challenging some basic assumptions about seniors’ listening needs and variability.
The focus of this article is to challenge the assumption of what it means to grow old today and how an emerging new group of consumers—commonly referred to as healthy agers—have listening demands that will challenge how we view hearing instrument technology. Given the importance of social networks, removing the barriers posed by hearing impairment has the potential to promote healthy aging.
There is probably no other group of individuals more subject to misconception and stereotype than the elderly population. Historically, society’s prevailing views of the elderly cast them as being either weak and helpless or cantankerous and feisty. Not long ago, pop culture vignettes of these stereotypes were everywhere. Who can forget Wendy’s argumentative Clara Pellar shouting “Where’s the Beef?” at the sight of a skimpy McDonald’s hamburger, or the infamous “Help! I’ve Fallen and I Can’t Get Up,” a staple of late-night television viewing for more than 20 years. Both commercials, which portrayed the elderly as somewhere between feeble-minded and grouchy, are etched into the brain of many Americans. Both notorious television spots are examples of how the elderly population have been traditionally viewed by other age groups. And it’s not too big of a leap to suggest that these stereotypes of the elderly, who comprise the largest caseload for most practices, are still pervasive among hearing healthcare professionals. Even today, when you mention elderly patients to a hearing care professional, you are likely to conjure images of wheel- chairs, pocket talkers, and squealing hearing aids with oversized manual volume controls.
The New Boomers
Rather recently, however, these stereo- types about the elderly have begun to slowly change. Thanks in large part to the marvels of modern medicine, individuals are not only living longer, but have far healthier and more active lifestyles, often into their 9th decade. Individuals who are turning 65 today comprise the very first generation in human history to live the entirety of their lives with antibiotics and vaccinations. Unlike past generations, who often witnessed firsthand the devastating effects of childhood infectious disease and early death, today’s elderly population approaches the market for healthcare solution in a much different way. Ubiquitously known as the Baby Boomer generation (those born between 1946 and 1960), this large group of individuals—10,000 of them turn 65 every day—is ushering in a new era of healthcare centered on healthy aging. By the year 2030, 20% of the population will be aged 65 or older.1
Although it is tempting to focus only on the Baby Boomer generation, healthy agers are comprised of individuals from all generations. It seems that everyone wants to live to the ripe old age of 100 and maintain the vim and vigor of a 45-year-old. The focus of this article is to challenge the assumption of what it means to grow old today and how an emerging new group of consumers—commonly referred to as healthy agers—have listening demands that will challenge how we view hearing instrument technology.
Healthy Aging Defined
Healthy aging is best defined as the ability to maintain optimal cognitive and physical functioning throughout an individual’s lifespan. It is the ability of people to live a safe, healthy, and socially inclusive lifestyle. Although individuals over the age of 65 are more likely to be diagnosed with chronic conditions such as diabetes, dementia, hypertension, and hearing loss, their outlook toward those conditions is far more optimistic than that of previous generations of elderly people.
The term “optimism” doesn’t begin to describe the positive outlook of many elderly as Tergesen2 found that 58% of respondents ages 75+ feel younger than their chronological age. That same survey, published in the November 30, 2014 issue of The Wall Street Journal, also showed that across five categories of well-being (purpose, social, financial, community, and physical), individuals over age 65 reported higher ratings than all other ages categories. Clearly, today’s elderly are much different than previous generations.
Although these findings from outside our own field suggest the final decades of one’s life to be vibrant, active and extremely fulfilling, they are somewhat contrary to some of the published evidence in the audiology literature. Several early studies have investigated the effects of aging on a hearing aid user’s auditory lifestyle. Studies by Kricos et al,3 Gatehouse,4 and Erdman and Demorest5 indicate that older adults tend to have fewer listening demands relative to their younger peers.
The most plausible explanation for this association between age and auditory lifestyle is that older adults have less active social lifestyles that place fewer demands on hearing. Furthermore, this link between age and auditory lifestyle may explain why older adults are less likely to prefer directional microphones6 and report fewer negative reactions toward background noise in everyday listening situations when wearing hearing aids.7
Recently, Wu and Bentler8 evaluated the auditory lifestyle and listening demands of 27 adults, ranging in age from 40 to 88. Analyzing journal entries and dosimeter readers, the researchers concluded that older listeners tend to encounter quieter listening situations and have less active social lifestyles that place fewer demands on hearing than those of their younger counterparts. Maybe those stereotypical images of the old man with the squealing hearing aid who simply needs to hear his wife and television are not too far off base?
Research from gerontology may dispel this myth and help us explain the discrepancy between higher levels of optimism and well-being, yet a less active social lifestyle in healthy agers. Wrzus et al9 conducted a meta-analysis of 277 studies for changing social networks across the lifespan. The authors concluded that, while both friendship and workplace networks steadily declined from young adulthood to old age, the overall importance of social networks did not diminish as people age.
English and Carstensen10 in 2014 observed that the number of peripheral relationships diminishes as individuals age, while the number of close friends is stable over a long period of time. Additionally, these researchers found that, as people age, they selectively narrow social networks, often resulting in improved emotional experiences in daily life.
Given the importance of social networks, removing the barriers posed by hearing impairment has the potential to promote healthy aging.11 It is imperative for the entire industry—manufacturers, suppliers, and clinicians alike—to critically evaluate how current implementations of various product features can better meet the demands of healthy agers.
The Healthy Aging Lifestyle
Taken together, this research may suggest that active older adults—even when placed in demanding listening situations—have simply gained perspective and are quite content to tolerate insufficient signal processing strategies. Beyond auditory lifestyle and listening demands, it is worth exploring other realms of the healthy aging experience to see if new implementations of hearing aid technology may be warranted. Compared to previous generations of the elderly, healthy agers possess three traits that should cause all hearing care professionals to pause and rethink how they can more effectively meet the needs of healthy agers.
A positive outlook on life. Contrary to the popular view that youth is the best time of life, Carstensen et al1 report that emotional well-being does not often peak until a person is well into their 8th decade of life. In this 15-year longitudinal study, emotional well-being was measured on adults ages 18 to 94. The conclusions of the authors were that, as participants aged, their moods steadily improved. In general, older adults tend to be happier, less angry, and socially more active than previously thought. This study is in alignment with the socioemotional selectivity theory of aging, which posits that, as we age, we strive to live in the moment, know what’s important, deepen relationships, and savor life—characteristics of the elderly that are a far cry from the frail bedridden lady in the “Clapper” commercials.
Cognitive activity contributes to open- mindedness. Society largely views the way that elderly think as slow, rigid, and outdated. And, of course, the elderly are more prone to cognitive decline resulting from various forms of dementia. However, there are threads of cognitive science research suggesting that certain cognitive skills are working at or near peak capacity in healthy agers.
Given their level of real-world experience, healthy agers with near-normal hearing actually do quite well on a number of cognitive tests. For example, Levy et al12 followed 396 participants over a 38-year period. Those with negative self-stereotypes of aging had a 30% decline in memory performance compared to those with positive stereotypes of aging.
Other research13 has shown that cognitively active participants ages 65+ have superior ability to see problems from multiple angles and show sensitivity in social relationships among groups of diverse individuals. In general, healthy agers exude practical wisdom and subtle reasoning skills that have only recently begun to be fully appreciated.
Productive and adaptable workers.
Today, 22% of the American workforce is comprised of people ages 55 and older—nearly double the number in 1992. Given the stereotype of older workers as slow and behind the times (recall Jerry Seinfeld’s dad, Maury, the raincoat salesman), it may seem somewhat surprising that many studies show no relationship between age and job performance.
Supan and Weiss14 studied the number and severity of errors in an automobile manufacturing assembly line over a 4-year period. The researchers determined that older workers committed fewer errors than their younger colleagues. Considering that nearly a quarter of the current workforce is 55 and older, the workplace may present an opportunity for the hearing industry to find better, more robust solutions to improve hearing and communication for this growing population of employees.
Listening Challenges of Healthy Agers
These three lines of research go a long way toward shattering many of the stereotypes associated with aging. They indicate that healthy agers lead much more vibrant and dynamic lifestyles than previously thought, even though they often report reduced listening demands. The conventional view that elderly patients lead sedentary lifestyles, which warrants a recommendation for basic or entry-level hearing aid technology is not supported by the evidence. Perhaps the hearing industry has underestimated the needs of our largest demographic—individuals over the age of 65 who have an inherent need to maintain optimal cognitive, physical, and social function over the final 3 decades of their lives.
Do Smaller Social Circles Lead to Reduced Hearing Demands?
Do the smaller social circles preferred by healthy agers also lead to less complex listening environments? To answer this question, we fitted 23 people with hearing aids during a typical new product validation. All the hearing aids relied on automatic programs that could recognize the type of acoustic environment in which the person was wearing them. The clinical validation sample was a good cross-section of healthy agers, as they represented a range of hearing losses and of ages (mostly retired). Additionally, they all tended to be healthy and ambulatory people who lead average lifestyles for their age. Below, we will discuss two good representative examples from this sample of healthy agers.
All of the hearing aids the participants wore had multi-destination automatic programs able to classify and match the usual 2, 3, or 4 listening destinations that are typical for commercially available hearing aids (although the aids were also capable of classifying up to 7 discrete listening environments at the same time). In other words, even though an instrument could switch automatically between two discrete listening programs such as quiet/noise, in the background it was also classifying all the acoustic environments with greater granularity into 7 different listening situations. These were (with examples in parentheses): 1) Quiet conversation (one on one, lecture hall); 2) Small group conversation (board meet- ing, dinner table); 3) Quiet listening (reading a book, walk- ing in the woods); 4) Large group conversation (busy restaurant, wedding reception); 5) Conversation in noise (talk radio in the car, conversation on bus or train); 6) Just noise (busy street, worksite); and 7) Music (instrumental, with singing).
The purpose of this research was to determine how many different listening destinations in which these people found themselves and to see how well the existing 2-, 3-, and 4-destination hearing aids suited the users’ needs. If these people truly were relatively sedentary and not particularly social (as the stereotypes would imply), then they should spend almost all of their time in quiet and fairly easy listening situations. The objective was to show the group results of all 23 participants. However, it quickly became apparent that their listening profiles contained so much individual variation that we had to look at their listening profiles and their needs individually.

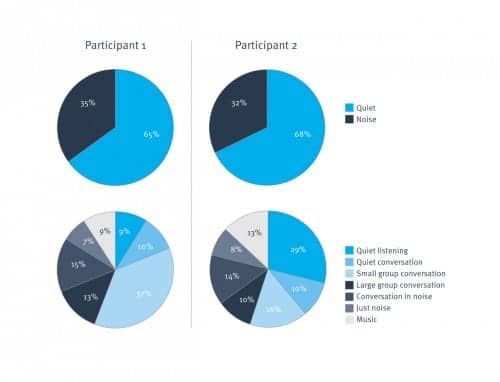
Figure 1. Results from two representative study participants and the classification of their listening environments. In the top two pie charts, using a 2-destination (quiet or noise) paradigm to classify their listening environments, one could be led to believe that they encounter very similar listening environments and have very similar listening needs. However, a more granular 7-item categorization of the listening environments (bottom two pie charts) reveals important differences for these two individuals.
Figure 1 shows two illustrative listening profiles with the percentage of time that each participant spent in various listening environments. The results for the first participant are on the left-hand side and the second participant on the right-hand side. The top two pie charts show how the hearing aids classified each person’s listening environments over a 3-week period of daily use for a typical 2-destination automatic program (quiet or noise). The bottom two sections of the figure show the more granular classifier results for the exact same 3-week period, but monitored with greater precision into the seven listening environments detailed above.
It is clear that the 2-destination automatic spent almost exactly the same percentage of time in quiet for each of the two participants (35% vs 32%). Of course, this means the noise environments were also nearly identical for these two people after 3 weeks of use (65% vs 68%).
The 7-environment classification shows that each participant spent a minimum of 7% of their time in every one of the 7 destinations. These two people are leading active, social, and nonsedentary lifestyles. Looking closer, it is clear that the distribution of listening environments is far more dissimilar for these two people than the 2-destination automatic hearing aids make it appear. Participant 1 was engaged in small group conversations 37% of the time, as opposed to only 16% (less than half as much) for Participant 2. Meanwhile, Participant 1 spent only 9% of the time in quiet with no speech; Participant 2 spent 29% (over 3 times as much) of the time in quiet listening.
The final observation worth mentioning from this example is that the two participants spent 9% and 13% of their time listening to music, respectively. Unlike the other 6 speech or noise destinations, music could not have been properly classified in the 2-destination automatic device. Music is neither speech nor noise. Thus, the correct listening environ- ment was certainly misclassified at least 9% or 13% of the time these people were wearing their 2-destination hearing aids.
Opportunities to Better Meet the Needs of Healthy Agers
This paper illustrates a few different points for hearing healthcare professionals with respect to healthy agers. For example, these two individuals, like most healthy agers, clearly do not spend all of their time sitting passively in quiet environments. In general, healthy agers operate in a wide range of listening environments with listening profiles that are unique to them.
Furthermore, all listening situations cannot correctly be boiled down to either speech or noise without significant misclassification and substandard performance. Using tools such as higher-precision classification could gain much greater insight into each hearing aid wearer’s personal condition. This would allow use of their own hearing aids to build a comprehensive listening profile specific to their experiences.
The possibility of utilizing such precise data clinically would allow hearing healthcare professionals to troubleshoot issues with a much greater cause-and-effect connection. Clinicians could even use the individual’s listening profile as a counseling tool while determining if the patient requires a higher or lower level of technology to provide the maximum value in their purchase and appropriately address all of their needs.
References
1. Carstensen L, Turan B, Scheibe S, et al. Emotional experience improves with age: evidence based on over 10 years of experience sampling. Psychol Aging. 2011;26(1):21-33.
2.Tergesen A. Why everything you know about aging is probably wrong. Dec 1, 2014. Wall Street Journal. Available at: http://www.wsj.com/articles/ why-everything-you-think-about-aging-may-be- wrong-1417408057
3. Kricos P, Erdman S, Bratt G, Williams D. Psychosocial correlates of hearing aid adjustment. J Am Acad Audiol. 2007;18(4):304-322.
4. Gatehouse S. Determinants of self-reported disability in older subjects. Ear Hear. 1990;11:57S-65S.
5. Erdman S, Demorest M. Adjustment to hearing impairment II: audiological and demographic correlates. J Speech Hear Res. 1998;41(1):123-136.
6. Wu Y. Effect of age in directional microphone hearing aid benefit and preference. J Am Acad Audiol. 2010;21(2):78089.
7. Cox R, Alexander G. The abbreviated profile of hearing aid benefit. Ear Hear. 1995;16(2):176-186.
8. Wu Y, Bentler R. Do older adults have social lifestyles that place fewer demands on hearing? J Am Acad Audiol. 2012;23(9):697-711.
9. Wrzus C, Hanel M, Wagner J, Neyer FJ. Social network changes and life events across the life span: a meta-analysis. Psychol Bull. 2013;139(1):53-80.
10. English T, Carstensen L. Selective narrowing of social networks across adulthood is associated with improved emotional experience in daily life. Intern J Behav Dev. 2014;38(2):195-202.
11. Weinstein B. On hearing loss and healthy aging. Hear Jour. 2014;67(12):6.
12. Levy BR, Zonderman AB, Slade MD, Ferrucci L. Memory shaped by age stereotypes over time. J Gerontol B Psychol Sci Soc Sci. 2012;67(4):432-436.
13. Grossmann I, Karasawa M, Kan C, Kitayama S. A cultural perspective on emotional experiences across the life span. Emotion. 2014;14(4):679-692.
14. Supan A, Weiss M. Productivity and age: Evidence from work teams at the assembly line. White Paper: Munich Center for the Economics of Aging (MEA) at the Max Planck Institute for Social Law and Social Policy; 2014.

Brian Taylor, AuD, is director of practice development and clinical affairs at Unitron, Plymouth, Minn.

Donald Hayes, PhD, is director of clinical research at Unitron world headquarters in Kitchener, Ontario, Canada.
Correspondence can be addressed to Dr Taylor at: [email protected]
Citation for this article: Taylor, B, Hayes, D. Does Current Hearing Aid Technology Meet the Needs of Healthy Aging? Hearing Review. 2015;21(2):22.